Occupational Health Managers Fighting the Spread of Coronavirus in Companies
By Chem. Eng. Raúl Escobar Márquez, FCIH
As we all know, the World Health Organization (WHO) has declared the coronavirus, also known as COVID-19, a matter of public emergency. The situation is serious and requires urgent strategies for its control, specially designed and applied for workers around the world. Thus, it is essential that directors of companies ask for the contribution of all the workers to avoid the spread of the virus. Especially from those in charge of Occupational Health in the company. As specified in the logical action process of industrial hygiene, the first factor to be analyzed is the general characteristics of the offending agent, in this case, THE CORONAVIRUS.
The Coronavirus
COVID-19 is part of the coronavirus family that causes various respiratory diseases, including acute respiratory distress syndrome (ARDS) and the common cold, usually affecting humans at the mid-level, although it is known to have caused severe illness in a minority of infected patients, and in some cases, death.
The virus that causes respiratory illness is typically spread through liquid droplets suspended in the air, which are sprayed by infected people when they cough or sneeze. They can be transported, deposited in the nose or mouth, and inhaled by physical means by other individuals. A person can transfer the coronavirus to their body if they breathe in the drops, or if they come into contact with a surface or object that has viral particles in it and touch their mouth, nose or eyes.
Where and how long does the virus live
According to specialists, the virus’s life span in the air is around 3 hours, and on common surfaces such as transport handrail tubes, stair handrails, and even money, depends on many factors. So it fluctuates in several hours a day.
Specialized studies have found that the virus can live 4 hours on copper, 1 day on cardboard surfaces, and up to 3 days on plastic or stainless steel, at room temperature. The coronavirus lives longer on stainless steel than on polypropylene and plastics used to make toys and auto parts.
Regarding the type of surfaces, non-porous smooth surfaces such as doorknobs are better transmitters, contrary to porous surfaces such as coins, hair or fabrics, where the virus needs to survive longer in the small holes that trap it before being transferred to other sites. Coins transmit the virus better than banknotes, however, they are considered low-risk transmitters since money is already handled with specific precautions given its origin and the number of hands it passes through. Glass and aluminum materials of cell phones can also carry viral particles.
Temperature is equally important in the life of the virus. COVID-19 has a lipid membrane, basically a layer of fat, that protects it from the outside world when it travels from person to person. But if there’s a temperature increase, let’s say from 20 ° C to 30 ° C, the air through which the virus is traveling dries up and with it, the virus dies. Therefore, the conditions of high humidity, moderate temperature and low wind on a solid surface favor the survival of the virus. This also explains why respiratory virus diseases are typically seasonal, therefore the protective layer and the life of the virus is preserved in cold temperatures.
Once the Coronavirus is on a surface, it is convenient to deactivate it with actions that favor its elimination, using the surface decontamination techniques that have been proposed, based on the application of mixtures of chemical products with ethanol, hydrogen peroxide or hypochlorite of sodium. The action time of these products is estimated to be from 15 seconds after application. However, to achieve greater efficiency, waiting some minutes after applying the products is required.
Symptoms
Regarding the physical response to the virus, it has been reported that generally, the symptoms of the disease caused by COVID-19 include fever, cough, and shortness of breath. These symptoms can appear from two days to two weeks after the initial exposure to the virus. Most people diagnosed have symptoms similar to a moderate common cold, however, risk increases with the age of each person. Also, a person with impaired health conditions or with immune deficiency (diabetics, hypertensive) is more prone to get stronger symptoms.
Risks for the working population
In countries where cases of infection have been identified, the entire working population is exposed to the risk of being infected. However, the probability of this happening is much higher in those workers who, due to their function, are in direct contact with infected people. Also, travelers returning from international locations where the disease is present have a higher probability of being infected.
After knowing the characteristics, the ways of acting, and the effects of the agent, industrial hygiene recommends developing 3 stages for its control:
Stage 1: Risk Recognition: Set of activities intended to define the level of workers’ exposure to conditions that could affect their health or well-being.
Stage 2: Risk assessment: Assessment of the probability that the agent negatively impacts the health or well-being of the people exposed to it.
Stage 3: Risk control: Defining the actions to be taken to minimize the level of risk identified and evaluated.
Actions for each stage
1. For the recognition of the risk: Derived from the possible random exposure of the workers or suspicion that they are infected as a consequence of acquiring the virus in the exterior (on their way to work, attending conglomerate places or through contact with an infected asymptomatic person), the following actions are recommended:
- Motivate workers to collaborate with your preventive program by explaining to them what is happening and asking them to strictly follow the instructions of health commissioners.
- Ask workers to avoid attending the workplace if they have any irregularity in their health or any cold symptoms. Instead, they should report it to you and schedule an appointment for an evaluation.
- Segment workers into groups. Identify which groups are more prone to be affected because of their age or physical condition.
- Identify workers who have recently traveled abroad or come into contact with people from abroad.
- Identify people who would have been in contact with someone suspected of being infected or infected.
- Measure body temperature (may be tympanic) at the beginning of every workday.
- Ask them to minimize direct person-to-person contact.
- Establish a respiratory protection system with the bases indicated below.
2. For Risk Assessment: For groups of workers without identified risk, unfortunately, there is no effective, practical and reliable environmental or biological indicator that can be assessed to measure the probability of being infected. For this reason, the only acceptable resource is to assess risk based on the information gathered in the recognition stage and thus be able to define how likely it is to affect these workers.
For workers that because of the job they perform, must handle people that could be infected or affected, it is a subject beyond the scope of industrial hygiene. Therefore, the participation of experts in the field is recommended.
- Take a specific training course taught by specialists to have a better understanding of the actions that can help minimize the probability of risk.
3. For the control stage: Industrial hygiene recommends minimizing the level of potential risk, through lines of an action directed at the causative agent, personnel and the form of exposure.
Recommendations
For managing the causal agent:
- Establish control systems to limit the entry of people from abroad who may be infected.
- Establish rules for managing people external to your business to minimize their contact with the personnel.
- Minimize the probability of the existence of the agent with sanitization procedures in the places with the highest frequency of personnel contact, especially on smooth surfaces.
For managing exposed personnel:
- Establish a specific surveillance system for personnel classified as vulnerable or at risk of transmission.
- Recommend specific actions that favor health and the immune system.
- Recommend social behavior that minimizes the probability of external infections.
For managing the exposure control phase:
- Minimize the probability of contact with the causative agent.
- Reduce the frequency of possible exposure to the causative agent.
- Minimize exposure times to the causative agent.
- Minimize the magnitude of exposure to the causative agent. The use of personal protective equipment is one of the necessary control alternatives for practical use. Also, keep in mind that a personal protection program for the respiratory tract is very useful, and will generate better results if it is implemented as established by the authorities fulfilling the following points:
The personal respiratory protection program
- It must have a person fully prepared for the promotion and evaluation of results.
- It must be formulated in writing and accepted by senior management.
- It must have an industrial hygiene study that indicates the level of risk and the characteristics of the exposure.
- It must assess the capabilities (physical, organic and of attitudes) of the users to guarantee their acceptance and use.
- Protection devices must be selected to guarantee the protection needed (in the best of cases with certification by an institution).
- They must have a procedure to train personnel for their proper use, conservation, replacement, and disposal.
- Personnel using it should be periodically evaluated to define their effectiveness.
- The daily use of the device and the acceptance by users must be continuously evaluated.
Occupational health managers are extremely important in companies because they are trained to carry out the process of controlling occupational risks from exposure to physical, chemical or biological agents such as COVID-19. Considering this, here are some recommendations on how they can contribute to the better management of this situation:
- Formulating and applicating the personal protection program.
- Training of personnel to follow up on preventive and personal protection recommendations
- Advice for the use of decontamination techniques and materials to use.
- Handling of waste materials, in the handling operations of suspicious or infected people.
- Establishing of policies and standards to follow for risk prevention and control.
- Understanding the characteristics and conditions of the risk caused by exposed or presumably exposed personnel.
- Programming of the work cycles of health employees.
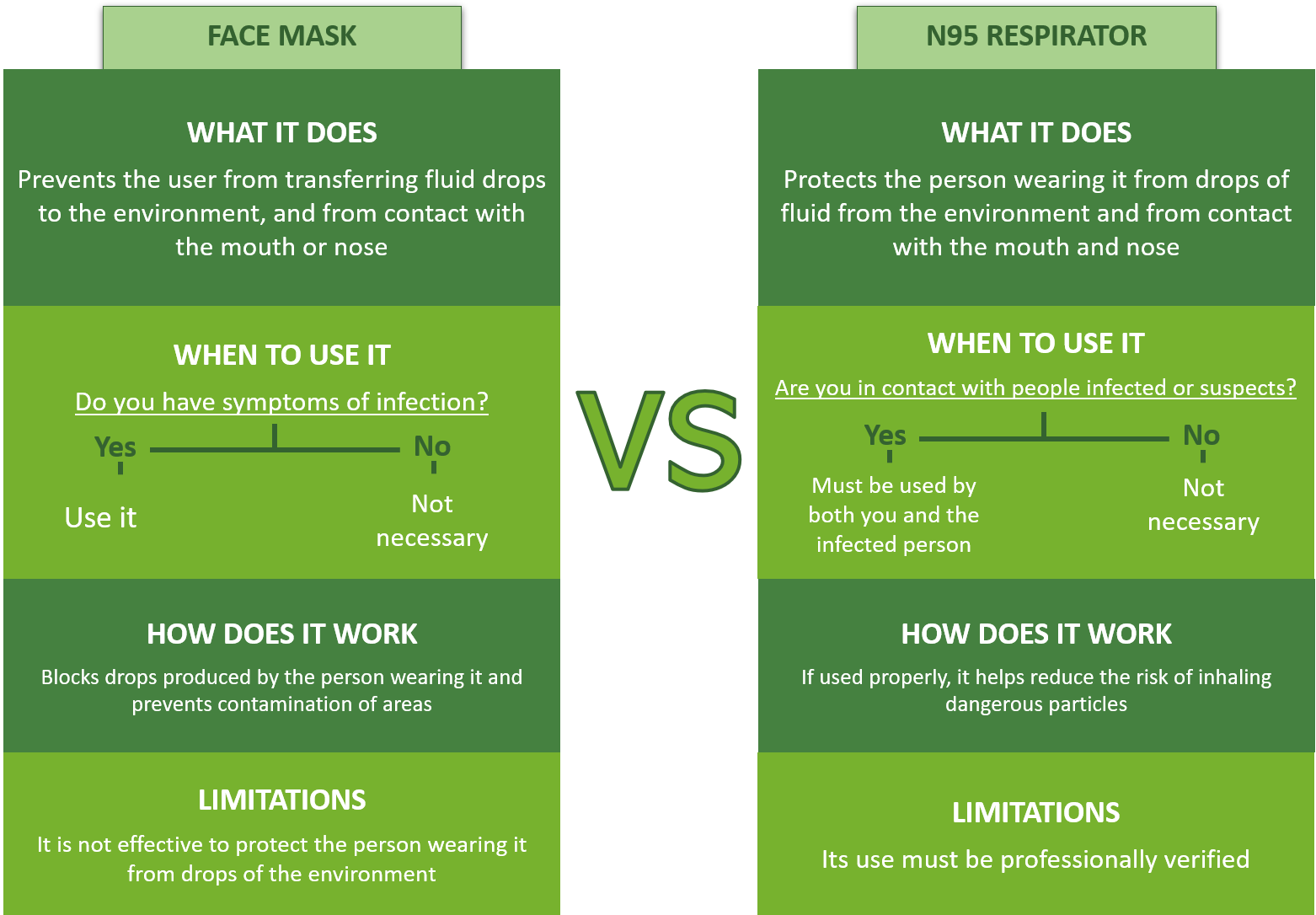
For your information, some general aspects of respiratory protection equipment are:
- Respiratory protection equipment is not recommended for permanent use since most of the affections occur rather by contact from person to person.
- The usual types of respiratory protection are those known as face masks and respirators.
- Face masks are recommended protection devices to prevent drops of fluid containing viruses from being sent into the environment while sneezing or coughing. Although these do not protect the person from getting the virus by air, it is still recognized that because it keeps you from touching your nose or mouth with your hands, it will lead to reducing the risk of entry by that route.
- Respirators are personal protection devices designed and approved by an institution to protect the person from the entry of polluted materials into their respiratory system. In the case of COVID-19, the respirator recommended by the United States is the one that belongs to the classification called N95.
- Respirators approved in the N95 class have been shown to retain particles down to 0.3 microns with 95% efficiency and are capable of stopping all types of particles including bacteria and viruses.